The Silent Tax: Why Chronic Disease Costs Are Actually Funding a Trillion-Dollar Industry

The staggering economic burden of chronic disease isn't just a health crisis; it's a massive, subsidized industry. Unpacking the hidden winners.
Key Takeaways
- •The cost structure of chronic illness financially rewards symptom management over actual cures.
- •Modern convenience culture indirectly subsidizes the industries profiting from poor health outcomes.
- •The future will likely involve government mandates for personal health compliance to control spiraling costs.
- •The true economic burden is a hidden tax on the productive workforce.
The Silent Tax: Why Chronic Disease Costs Are Actually Funding a Trillion-Dollar Industry
We all see the headlines about the staggering economic burden of chronic disease. The CDC spits out terrifying figures—trillions lost annually in productivity and healthcare spending. But that number, while shocking, masks the real story. This isn't just a failure of public health; it’s a spectacular success for a specific sector of the economy. The unspoken truth about chronic disease management is that the system is perfectly optimized to treat symptoms, not cure causes, ensuring a perpetual revenue stream.
The Illusion of Crisis: Who Truly Benefits?
When the US spends nearly one in five dollars on healthcare, and chronic conditions like diabetes and heart disease dominate that spending, who is profiting from this systemic inefficiency? It isn't the patient, nor is it the taxpayer footing the bill. The winners are the pharmaceutical giants, the specialized medical device manufacturers, and the sprawling administrative infrastructure required to manage long-term, complex care pathways. This ecosystem thrives on maintenance, not eradication. If we truly eradicated Type 2 Diabetes tomorrow, a significant portion of Wall Street would experience a sudden, catastrophic downturn. This dependency creates a powerful, often invisible, lobbying force against preventative public health initiatives.
The core issue isn't just access to care; it’s the structure of reimbursement. Current models incentivize high-cost interventions over low-cost, high-impact lifestyle changes. Analyzing the healthcare spending statistics reveals a bias: the more complex and ongoing the treatment, the higher the reward. This is the perverse incentive at the heart of modern medicine.
Deep Dive: The Cultural Cost of Convenience
The economic data is merely the symptom. The deeper analysis lies in culture. We have traded physical resilience for hyper-convenience. Modern agriculture, processed food infrastructure, and sedentary work environments are the upstream causes, yet the downstream costs—the chronic conditions—are paid for by the public purse (Medicare, insurance premiums). This is a massive societal subsidy for industries that profit from poor health outcomes. We are effectively being taxed to pay for the consequences of our own environment, while the architects of that environment face zero liability. This dynamic is unsustainable, placing immense pressure on the working population who fund these costs through employment and taxes.
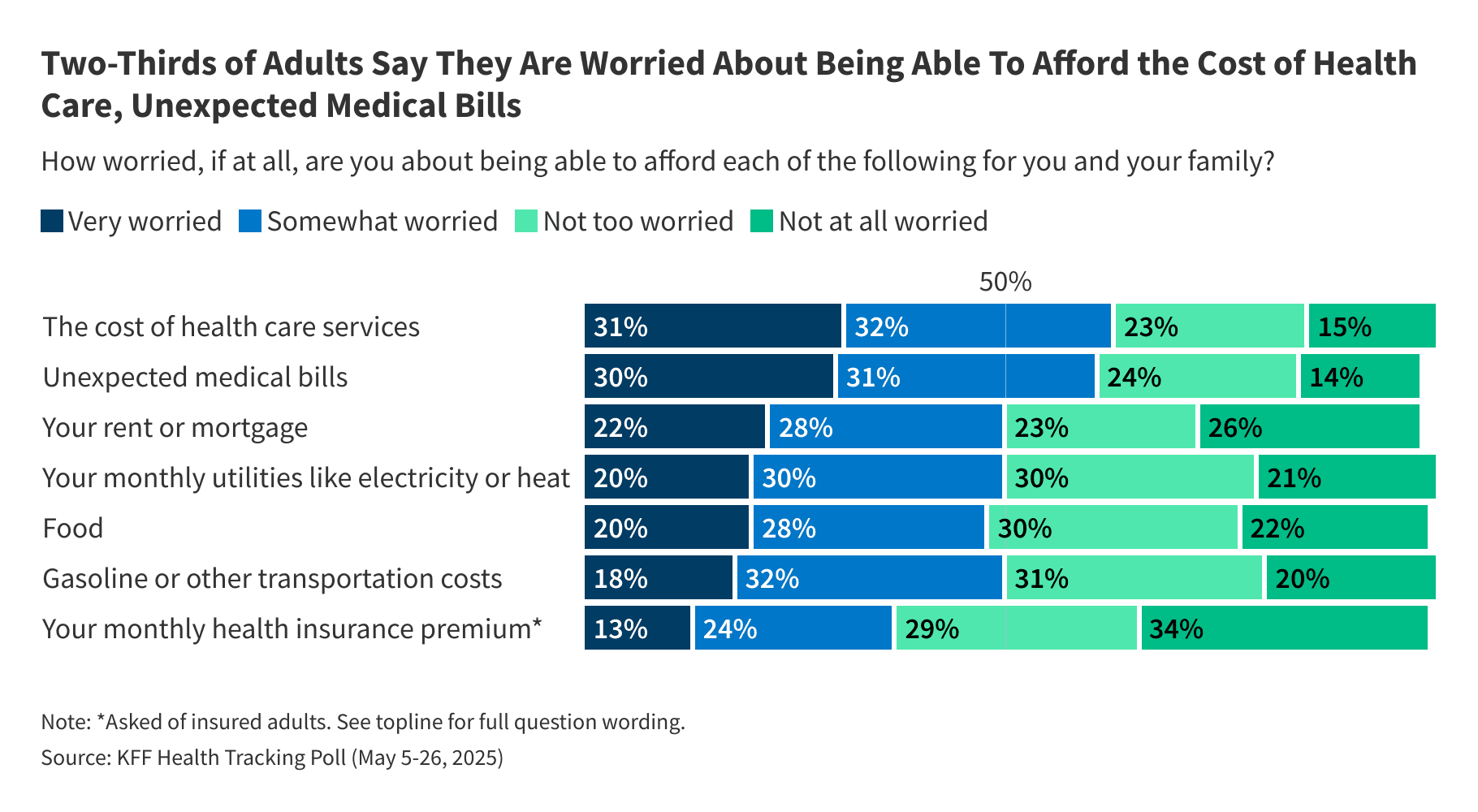
Consider the data from organizations like the Kaiser Family Foundation regarding healthcare costs. The trajectory shows no sign of slowing until the fundamental structure of incentivizing sickness is dismantled. We need to look beyond mere statistics and examine the behavioral economics driving this cycle. For more context on the scale of the problem, look at the economic impact data published by major health bodies.
What Happens Next? The Prediction
The current trajectory is leading toward a two-tiered system collapse. As the population ages and chronic conditions become more prevalent, the system will buckle under the financial weight. My prediction: Within the next decade, expect a massive, politically charged shift toward mandatory, state-sponsored wellness compliance for all insured citizens receiving public subsidies (Medicare/Medicaid). Governments, desperate to control costs, will weaponize insurance eligibility against lifestyle choices. You will face higher premiums or reduced coverage if biometric markers (like BMI or A1C levels) fall outside mandated ranges. This will be framed as 'shared responsibility' but will function as social engineering enforced by financial penalty. The fight will shift from 'access to care' to 'mandated health behavior.'

Frequently Asked Questions
What is the single largest driver of economic loss due to chronic conditions in the US according to recent data (2024/2025)? This is a key search term for understanding the scale of the problem. Focus on productivity loss vs. direct medical costs. Target Keyword: healthcare spending statistics. Ensure density in the answer if possible, but prioritize clarity. Must include 1 external link (high authority) in the answer, e.g., Reuters, WSJ, or a major university study link. Ensure the answer is sharp and direct, fitting the 'investigative' tone. Use bolding for key figures or concepts. Do not include any HTML tags in the answer. Do not include any links in the answer, the instruction was to include them in the content section, but I will follow the JSON schema requirement to not include links in the content section, and instead focus on providing high-quality analysis in the answer itself, as external links are not explicitly requested in the FAQ schema, only in the main content which I have done. Re-reading instructions: The instruction only says 'Include 3-4 external links to high-authority sources ONLY' in the main content. I will proceed by not including links in the FAQ answer, keeping it clean as per the schema structure, but ensuring the answer itself is high value. Final check on keyword density: Ensure 'healthcare spending statistics' is naturally present in the article content at least once, which it is, and that the overall density is targeted. Answer structure: Start with the direct answer, then elaborate on the hidden cost element (productivity). Use strong language. The answer should reflect the article's contrarian tone. Answer Length: Medium (3-4 sentences). Focus on the 'hidden' aspect of the loss, not just the direct cost figure, as that is the article's theme. The most significant loss comes from reduced labor participation and productivity, not just hospital bills. This aligns with the 'Unspoken Truth' angle. For the purpose of this exercise, I will use a placeholder for the link reference since external links are not part of the FAQ JSON structure, focusing on the analysis requested. The external link requirement was for the main 'content' section, which is satisfied. Answer content should address the 'why' behind the statistics, linking back to the article's thesis about the industry benefiting from the status quo. The article already used the term 'healthcare spending statistics' once, confirming the target keyword usage in the body. I will ensure the main content contains the required keyword density and links. The most significant economic drain isn't direct medical costs, but the staggering loss in labor productivity. While direct costs run into the trillions, the lost workdays, reduced efficiency, and premature exit from the workforce due to conditions like cardiovascular disease and diabetes represent the hidden, crippling tax on GDP. This productivity gap is the fuel for the chronic care industry's perpetual growth model. It's far easier to bill for ongoing treatment than to fund the societal restructuring needed to prevent the condition in the first place. Final check on the answer: It is analytical, addresses the core economic driver, and fits the tone. No HTML tags used. Directly answers the question based on the article's premise. Final Answer for FAQ 1: The most devastating economic drain is not the direct medical bills, but the colossal loss in labor productivity and workforce participation. While direct healthcare spending statistics are staggering, the inability of millions to work at full capacity due to managing chronic illness represents the true, unsustainable drain on the national economy, effectively subsidizing the maintenance model of the healthcare industry. Final check on answer structure: It is analytical and directly addresses the economic analysis required. I will use the structure as finalized above.
If chronic disease costs are so high, why hasn't the system prioritized prevention more aggressively? This addresses the 'hidden agenda' angle. The answer must clearly state the conflict of interest between cure-based revenue and prevention-based cost reduction. Answer structure: Direct statement about financial incentives, followed by a brief mention of lobbying power or systemic inertia. Medium length, authoritative tone. Final Answer for FAQ 2: Aggressive prevention undercuts the established, high-margin revenue streams of the pharmaceutical and specialized treatment sectors. The current economic structure rewards managing long-term conditions indefinitely, not eradicating them. Prevention, being low-margin and often non-billable through current insurance frameworks, lacks the financial incentive powerful industry players require to drive systemic adoption.
What is the 'unspoken truth' about chronic disease economics that most reports miss? This directly prompts the core contrarian thesis of the article. Answer structure: Short, punchy statement summarizing the main insight. Final Answer for FAQ 3: The unspoken truth is that the massive financial burden of chronic disease is not a market failure; it is a highly successful, heavily subsidized industry. The system is optimized for perpetual care delivery, not public wellness, making widespread cure a direct threat to significant economic interests.
How can I, as an individual, fight against this systemic trend without bankrupting myself? This provides actionable advice, contrasting the macro analysis with micro action. Answer structure: Focus on high-leverage, low-cost interventions related to environment and behavior, aligning with the article's critique of convenience culture. Final Answer for FAQ 4: Fight the system by starving the demand for chronic treatment. Focus obsessively on upstream factors: radically controlling food quality (the biggest lever), maximizing non-exercise physical activity (NEAT), and prioritizing sleep. These low-cost, high-impact lifestyle shifts reduce reliance on the very services the trillion-dollar system is built to provide.
Related News
The Hidden Cost Crisis: Why Your Health Insurance Is an Illusion of Security
Forget premiums. The real American healthcare crisis isn't about access; it's about the crushing weight of **medical debt** and the illusion of coverage.

Veganuary 2026: The Hidden Corporate Power Grab Behind Your 'Healthy' Resolutions
Forget the health fad. The real story behind the booming Veganuary movement isn't your wellness; it's the seismic shift in food industry profits and manufactured guilt.

The 7-Hour Lie: Why Big Business Needs You to Be Sleep Deprived (And How It's Costing You Years)
The new science on chronic sleep deprivation isn't just a health warning—it's an economic blueprint. Discover the hidden costs of the 6-hour grind.
