The Hidden Cost of Robotic Surgery: Why NYC's 100th Robotic Bronchoscopy Isn't the Victory They Claim

NYC Health + Hospitals celebrates a milestone in **robotic-assisted bronchoscopy**. But behind the PR spin lies a critical debate on medical technology adoption and cost.
Key Takeaways
- •The celebration masks the significant capital and recurring costs of high-end robotic systems within public health budgets.
- •The adoption rate suggests prestige and competitive pressure are driving procurement more than pure community need analysis.
- •The next step will be rapid proliferation across other large hospital networks, standardizing the high-cost procedure.
- •This incident highlights the ongoing tension between cutting-edge innovation and accessible primary care funding.
The Unspoken Truth: Celebrating 100, Ignoring the Bill
The press release from NYC Health + Hospitals/Jacobi touting their 100th case using the Ion **robotic-assisted bronchoscopy** system sounds like a triumph of public health. A century of minimally invasive lung biopsies—a clear win for patient outcomes, right? Wrong. This milestone isn't just about clinical proficiency; it’s a textbook case study in how high-cost, venture-backed medical technology infiltrates public hospital systems, often disguised as urgent necessity. The real story isn't the 100th procedure; it's the **medical technology** adoption curve. Robotic systems, like the Ion, promise superior navigation and access to peripheral lung nodules, crucial for early cancer detection. This capability is undeniable. However, the unspoken truth lies in the economics. These systems carry massive upfront capital costs and recurring proprietary supply expenses. For a system like NYC H+H, which operates on razor-thin margins serving vulnerable populations, every dollar spent on a cutting-edge robot is a dollar not spent on staffing, primary care infrastructure, or reducing wait times for basic screenings. Who truly wins? The manufacturer, who secures a foothold in a major metropolitan public health network, creating a standard of care that competitors must then match.Deep Dive: The Standardization Trap
Why does this matter in the grand scheme? We are witnessing the rapid **standardization** of elective or high-end procedural care over essential public health measures. The drive for institutional prestige—being the first, or reaching a round number fastest—often dictates procurement budgets more than community need assessments. While early detection via improved bronchoscopy is vital, we must ask: How many basic diagnostic tools could have been purchased for the cumulative cost of this robotic platform and its specialized consumables? This isn't about denying patients the best care; it’s about ensuring the *best* care isn't exclusively defined by the flashiest gadget. Compare this adoption speed to the often glacial rollout of proven, low-cost interventions in community clinics. The imbalance is stark.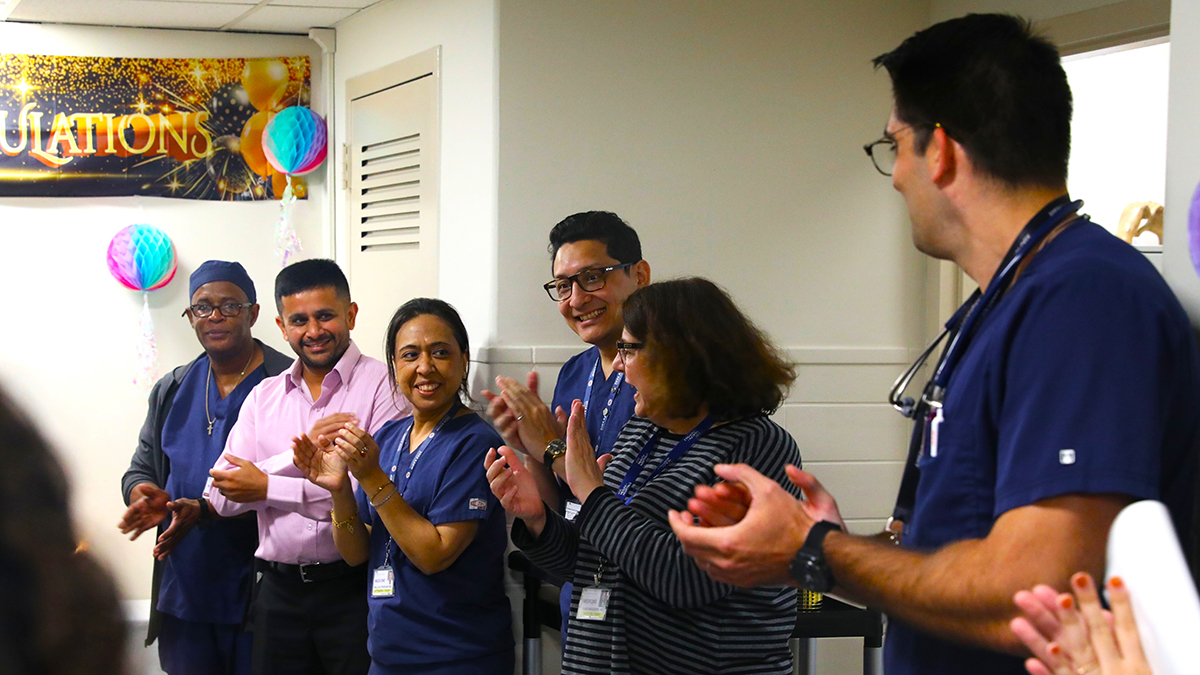
What Happens Next? The Inevitable Expansion
My prediction is that this 100-case milestone serves as the necessary proof-of-concept for expansion. Expect other major municipal and regional hospital systems to aggressively pursue the Ion or its competitors within the next 18 months. Once one major public system validates the technology's clinical utility (and absorbs the initial training costs), the pressure to adopt becomes immense—a classic 'keeping up with the Joneses' scenario in healthcare. Furthermore, watch for insurance providers to begin mandating robotic assistance for specific diagnoses within five years, effectively squeezing out centers unwilling or unable to invest, regardless of their existing surgeon skill levels. The future of pulmonary diagnostics will be roboticized, but the resulting financial strain on public health budgets will be the next crisis nobody wants to discuss. This trend reflects broader issues in American **healthcare innovation**, favoring capital-intensive solutions over scalable, accessible ones. For more on the economics of medical devices, examine reports from organizations tracking capital expenditure in the sector [link to a major financial news source like Reuters or WSJ on medical device markets]. The debate over value in medicine is far from settled.Frequently Asked Questions
What is Robotic-Assisted Bronchoscopy (Ion)?
It is a minimally invasive procedure that uses a flexible robotic catheter guided by advanced imaging (like CT scans) to reach and biopsy small, hard-to-reach nodules deep in the lungs, significantly improving early lung cancer detection rates.
Why is this technology controversial in public hospitals?
The controversy stems from the high upfront cost and ongoing proprietary supply costs associated with robotic platforms, which divert limited public funds from other essential, high-volume primary care services.
How does this compare to traditional bronchoscopy?
Traditional bronchoscopy relies on the physician's manual dexterity to navigate airways. Robotic assistance offers greater stability, precision, and reach into the periphery of the lung, increasing the diagnostic yield for small lesions.
Related News

The Digital Health Mirage: Why Patient-Centric Tech Hides a Corporate Data Grab
Digital health tools promise patient empowerment, but the real story behind this 'revolution' in **healthcare technology** is far more complex and corporate.
The AI Trojan Horse: Why Nurses Using ChatGPT is the Quiet Crisis for Patient Trust
Nearly half of nurses use AI, but the real story isn't efficiency—it's the erosion of the human element in healthcare.

The WHO's Digital Playtime Trap: Why 'Social Health' Is Just New Code for Digital Control
The WHO's 'Social Health' talk masks a deeper battle over digital literacy and corporate power in youth mental health.

DailyWorld Editorial
AI-Assisted, Human-Reviewed
Reviewed By
DailyWorld Editorial