The Ōamaru Tragedy: Why Understaffing in Aged Care Is a Deliberate, Profitable Policy, Not a Mistake
The death of an elderly woman in Ōamaru due to poor staffing isn't a tragedy; it's the predictable outcome of a broken system. Analyze the hidden costs of cheap care.
Key Takeaways
- •The Ōamaru death is a predictable outcome of a profit-driven model in aged care, not an isolated incident.
- •Current funding structures actively incentivize running facilities below safe staffing thresholds to maximize returns.
- •The long-term trend will be corporate consolidation and substitution of human care with technology.
- •The core issue is the commodification of vulnerable elderly citizens within the New Zealand healthcare framework.
The Hook: When Negligence Becomes the Business Model
We are fed the soothing narrative: the Ōamaru incident, where an elderly woman died due to what is being politely termed poor staffing in aged care, is an unfortunate anomaly. A regrettable failure of process. This is a lie. This isn't a staffing crisis; it is the logical, inevitable conclusion of a decade-long economic strategy prioritizing shareholder returns over human dignity. The real scandal isn't the single death; it’s the systemic acceptance of this calculated risk across the entire aged care sector.
The key question nobody in the mainstream is asking about this New Zealand healthcare failure is: Who benefits from running facilities so lean that inevitable fatalities become acceptable collateral damage? The answer is invariably the corporate owners who view the government subsidies as revenue streams, not trust funds for patient welfare.
The 'Meat': Deconstructing the Staffing Scapegoat
Reports citing the Aged Care Commissioner point fingers at inadequate staffing ratios. This is surface-level analysis. The deeper truth is that the current funding model *incentivizes* understaffing. Why hire an additional registered nurse when a lower-paid care assistant, working longer hours, can theoretically cover the gap? The gap, of course, manifests in overlooked call buttons, delayed medication, and, ultimately, preventable deaths.
This isn't just about Oamaru; it’s a national epidemic of austerity disguised as efficiency. When staff turnover skyrockets because the work is unsustainable—physically and emotionally—the cost of constant retraining is still less than paying competitive wages or maintaining safe ratios. We are witnessing the financial engineering of neglect. The underlying keyword here, **aged care sector**, is bleeding resources while political bodies debate marginal funding increases that fail to address the core profitability mandate.
The 'Why It Matters': The Commodification of Eldercare
The commodification of eldercare turns vulnerable citizens into line items on a balance sheet. When a facility is owned by a large entity, the pressure to maximize returns from fixed government funding becomes immense. This death forces a brief public reckoning, but the structural damage remains. We are outsourcing our moral obligation to the lowest bidder. This trend mirrors similar crises seen globally, where private equity sees aging populations as a guaranteed, inelastic market. The failure in Ōamaru is not a human resources error; it is a market signal that the current price point for care is dangerously low.
Future Prediction: The Inevitable Consolidation and Digital Overlord
What happens next? Expect a wave of mandatory, often performative, reviews. However, the true trajectory is towards further consolidation. Smaller, marginally compliant facilities will fold, bought out by larger chains who can absorb fines and leverage economies of scale (i.e., further cutting staff-to-patient ratios nationwide). Furthermore, expect a massive push for technological 'solutions'—remote monitoring, AI check-ins—to replace human interaction entirely. This digital veneer will be sold as 'modernizing **New Zealand healthcare**,' allowing operators to claim oversight while drastically reducing on-site human presence. The next death will be blamed on a software glitch, not a shortage of compassionate hands.
For a deeper look into systemic failures in healthcare funding, see analyses from organizations like the OECD regarding public expenditure priorities [https://www.oecd.org/health/]. The history of underfunding public services often follows predictable patterns [https://www.britannica.com/topic/public-sector-economics].
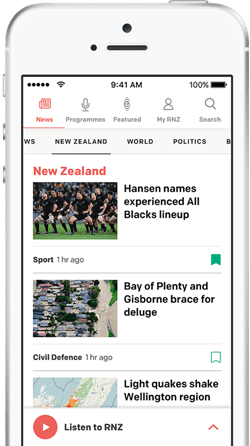
Gallery

Frequently Asked Questions
What is the current minimum staff-to-patient ratio for aged care in New Zealand?
New Zealand does not currently mandate strict minimum staff-to-patient ratios across the board, relying instead on facility-level assessments of resident needs, which critics argue is easily manipulated under financial pressure.
Who regulates aged care facilities in New Zealand?
Aged care facilities are primarily regulated by the Te Whatu Ora (Health New Zealand) system, with oversight functions provided by bodies like the Health and Disability Services Complaints and Advocacy Service.
Why is staffing so difficult in the aged care sector?
Recruitment and retention are hampered by low pay, high emotional and physical demands, insufficient training pathways, and a general lack of societal value placed on care work, leading to burnout and high turnover.
What is the main criticism of private ownership in aged care?
The main criticism is that private, often corporate, ownership introduces a fiduciary duty to shareholders, which can conflict directly with the duty of care to residents when cost-cutting measures are implemented.
Related News

The MRFF Grant Illusion: Who Really Wins When Billions Are 'Invested' in Medical Research?
The latest Medical Research Future Fund (MRFF) grant recipients are announced, but the real story behind this massive health funding shift is about political capital, not just cures.

The 15 Drugs Trump Picked: Why Medicare Price Negotiation Is A Political Weapon, Not Just Policy
The new Medicare drug price negotiation list isn't about saving seniors money; it’s a calculated political strike against Big Pharma.

Gracie Gold’s New Role Exposes the Toxic Lie Behind Olympic Mental Health
Figure skater Gracie Gold pivots to mental health advocacy, but the real story is the system's failure to protect elite athletes.
