The 70% Cancer Survival Myth: Who Really Profits From This 'Milestone'?

The US celebrates 70% cancer survival, but this headline masks a brutal truth about access, cost, and the 'forgotten' diagnoses.
Key Takeaways
- •The 70% survival rate is statistically skewed by highly treatable cancers, masking stagnation in aggressive forms.
- •The real winners are pharmaceutical companies, as high survival rates justify premium pricing for novel therapies.
- •A critical focus is missing on the long-term quality of life and chronic care needs of survivors.
- •Future progress hinges on economic pressure forcing a pivot towards preventative screening over expensive late-stage cures.
- •The Unspoken Truth Behind the 70% Cancer Survival Rate
- -The Statistical Mirage: Which Cancers Are Driving the Numbers?
- -Who Really Wins When Survival Hits 70%?
- -The Contrarian View: The Hidden Cost of Longevity
- -What Happens Next? The Prediction for Cancer Care
- -The Next Frontier: Personalized Medicine vs. Public Health
The Unspoken Truth Behind the 70% Cancer Survival Rate
We are being sold a narrative of relentless triumph. The news flashes that US cancer survival rates have hit a historic high of 70%—a seemingly unassailable victory banner waved over the American healthcare complex. But peel back the celebratory veneer, and the story shifts from medical miracle to economic dissection. This 70% figure, while numerically impressive, is a statistical sleight of hand that obscures profound systemic failures. It’s a fantastic number for PR, but a misleading metric for true public health progress. This isn't just about science; it's about access, equity, and the ruthless prioritization of certain diseases over others.

The Statistical Mirage: Which Cancers Are Driving the Numbers?
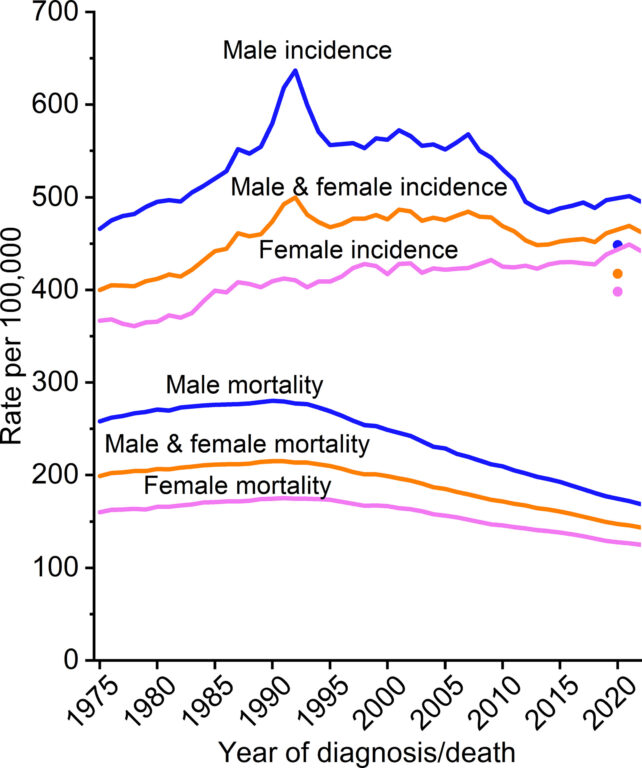
The headline screams 'cancer,' but the reality is siloed. This 70% milestone is overwhelmingly propped up by dramatic improvements in cancers that are often caught early or highly treatable, like prostate, breast, and early-stage colorectal cancers. These are the 'easy wins' that skew the average. What about the cancers that remain intractable—pancreatic, glioblastoma, or aggressive lung cancers? For millions battling these forms, the survival rate hasn't budged an inch. The critical keyword here isn't just cancer survival; it's disparity. The gap between the survival rates of the affluent, insured patient and the uninsured or underinsured patient accessing cutting-edge therapies is widening, not shrinking. This celebration conveniently ignores the socio-economic stratification of longevity.
Who Really Wins When Survival Hits 70%?
The primary beneficiaries of this headline are not the patients who will inevitably face the next diagnosis, but the pharmaceutical giants and the highly specialized oncology centers. A higher survival rate justifies higher prices for novel, often multi-hundred-thousand-dollar treatments. This success story fuels the engine of medical innovation, but it also solidifies the cost structure of American healthcare. The system is incentivized to create blockbuster drugs for high-profile, high-reimbursement cancers, rather than investing equally in population-level screening or palliative care for the less profitable diagnoses. We must analyze the economics of oncology research alongside the clinical outcomes.
The Contrarian View: The Hidden Cost of Longevity
We celebrate living longer with cancer, but what is the quality of that extended life? Aggressive, long-term chemotherapy and radiation regimens, while extending survival, often leave survivors grappling with chronic, debilitating side effects—neuropathy, secondary cancers, and profound fatigue. The healthcare infrastructure is excellent at treating the acute phase, but woefully inadequate at managing the chronic aftermath. This is the hidden cost of the 70% metric: a burgeoning population of long-term survivors requiring lifelong, expensive supportive care that often falls outside standard oncology billing codes. The focus on the 'cure' blinds us to the decades of complex survivorship.
What Happens Next? The Prediction for Cancer Care
The next major inflection point will not be a new drug, but a regulatory and economic reckoning. As the population ages, the burden of managing long-term cancer survivors will become fiscally unsustainable under the current model. Prediction: We will see a significant, albeit slow, pivot away from purely curative, high-cost interventions for certain late-stage cancers toward sophisticated, preventative genomic screening and aggressive early intervention models (like liquid biopsies). The industry will be forced to justify the ROI of treatments that offer marginal survival gains at astronomical costs. Expect major insurance companies to aggressively challenge reimbursement for therapies that do not demonstrate clear, cost-effective quality-of-life improvements alongside survival metrics. The era of unquestioning acceptance of high-cost cancer drugs is nearing its end, driven by pure fiscal necessity, not altruism. For more on the history of medical breakthroughs, see the timeline on Reuters.
The Next Frontier: Personalized Medicine vs. Public Health
The true measure of success will be whether we can translate these high-end successes into equitable public health outcomes. The data shows that improvements in cancer treatment are highly correlated with access to specialized academic centers, which are not available to rural or low-income populations. Until we solve the distribution problem—the 'last mile' of healthcare delivery—the 70% figure will remain a national success story for the privileged few, not a genuine benchmark for the nation. Read more about global health statistics from the World Health Organization to see the global context.
Gallery



Frequently Asked Questions
What specific cancers primarily contribute to the 70% US cancer survival rate?
The significant increase is largely driven by marked improvements in survival rates for prostate, breast, and early-stage colorectal cancers, which are often easier to detect and treat successfully.
Is the 70% survival rate the same for all demographics in the US?
No. There are significant disparities. Survival rates are consistently higher for affluent populations with better access to specialized care, early screening, and cutting-edge clinical trials compared to low-income or rural populations.
What is the 'hidden cost' of increased cancer survival rates?
The hidden cost is the long-term burden of chronic side effects from aggressive treatment, leading to a growing population requiring expensive, long-term supportive care that the current healthcare system is ill-equipped to manage affordably.
What is considered the next major challenge in cancer research?
The next challenge is shifting focus from incremental survival gains in late-stage disease to developing cost-effective, population-wide preventative genomic screening and improving the quality of life during survivorship.
Related News

The Exercise Lie: Why Your Daily Workout Is Failing You (And Who Benefits From The Confusion)
The latest science on fitness debunks decades of dogma. Discover the hidden agendas behind modern 'wellness' and the true path to longevity.

The Invisible Power Brokers: Why Biostatisticians, Not Doctors, Are Secretly Running Modern Medicine
The hidden truth about medical research isn't the drug, it's the math. Unmasking the biostatisticians driving clinical trial outcomes.
The Wind Chill Lie: How Weather Metrics Manipulate Your Perception of Risk
Forget the thermometer. The truth about **wind chill science** reveals a hidden agenda in how we interpret dangerous cold. This isn't just about safety.

DailyWorld Editorial
AI-Assisted, Human-Reviewed
Reviewed By
DailyWorld Editorial